Introduction
Chronic myeloid leukemia (CML) is a hematological malignancy with an excellent outcome. After advancements in CML treatment and the introduction of different Tyrosine kinase inhibitors (TKI), their life expectancy is equivalent to the normal population. As a result of that, coronary artery disease is anticipated to be the leading cause of death among CML patients. It was particularly noted that TKI use is associated with the risk of endothelial dysfunction and it associated risk of cardiovascular events, including myocardial infarction. In this study, we compare the outcome of PCI in patients with CML to their matched non-CML group.
Method
The National readmission database (NRD) was searched from January 2016 to December 2020 for the study population. Adults above (age ≥ 18 years) with chronic myeloid leukemia hospitalized with a primary diagnosis of myocardial infarction, ST Elevation Myocardial Infarction (STEMI), and Non-ST-elevation myocardial infarction (NSTEMI) were identified using ICD 10 code. The primary outcomes were in-hospital mortality and 30-day readmission, and the secondary outcome was to compare the complications. The weighting of patient-level observations was implemented to obtain national estimates. Multivariate regression analysis models were built by including all confounders significantly associated with the outcome on univariable analysis with a cutoff P-value of 0.2. Variables deemed important determinants of the outcomes based on literature were forced into the models. For readmission comparison, we used the time-to-event Cox regression analysis. Propensity matching was done by the Greedy method. Proportions were compared using the Mantel-Haenszel Chi-square test or Fisher exact test, and continuous variables were compared using the Student t-test. All P values were two-sided, with .05 as the threshold for statistical significance.
Results
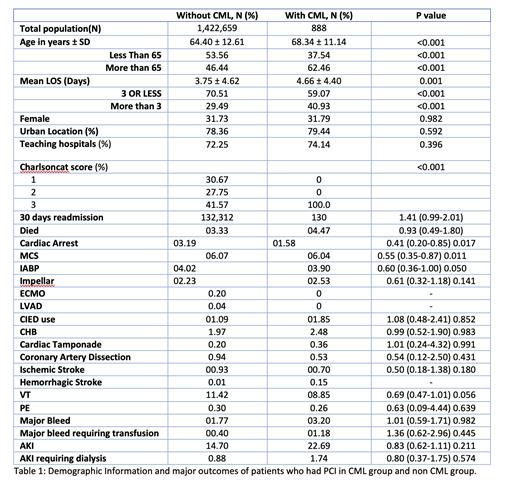
Out of 2727619 patients with myocardial infarction, 2124 CML patients were identified, and 888 CML patients had Percutaneous Coronary Intervention (PCI). Patients' baseline characteristics and major outcomes were compared (table 1). The mean age of CML patients was 68.34 ± 11.14 (P<0.001). The analysis showed no significant difference between CML and non-CML patients after PCI for the primary outcome of death 0.93 (CI 0.49-1.80) P value 0.527 and 30 days readmission rate 1.41 (0.99-2.01) P value 0.056. Also, there was no statistical significance in developing major complications, including cardiac arrest, coronary artery dissection, cardiac tamponade, stroke, thrombosis, major bleeding, AKI, and dialysis.
Discussion and Conclusion
Patients with hematologic malignancies, including chronic myeloid leukemia, are at increased risk of thrombosis. In CML, thrombosis can be venous or arterial (myocardial infarction, cerebrovascular accidents, and peripheral artery disease). Arterial thrombosis in CML is primarily linked to using different TKIs, and thrombotic events were reported with the second-generation TKIs like nilotinib, dasatinib, and ponatinib more often than with first-generation TKIs. The mechanism of TKI use-associated thrombosis is likely related to TKI-associated endothelial dysfunction and vascular toxicity that lead to accelerated atherosclerosis and subsequent vascular thrombosis. This increased risk might lead to an assumption of an increased risk of complications with vascular intervention like PCI. Some studies showed that PCI for hematological cancer patients with STEMI have no significant difference regarding in-hospital mortality. This analysis of patients with CML with myocardial infarction ( STEMI and NSTEMI ) showed no statistically significant difference in outcome after PCI between the two groups. There were no significant differences in mortality, 30 days readmission rate, and other complications post PCI. Therefore, diagnosis of chronic myeloid leukemia shouldn't prevent patients from receiving routine therapy and intervention because of the theoretical risk of thrombosis. This information aid in patient counseling and achieving the objective of maintaining a normal quality of life for chronic myeloid leukemia patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal